Factors which Influence the Frequency of Cognitive Assessment in the Emergency Department
Article information
Abstract
Background
The practice of safe emergency medicine requires accurate and adequate assessments. However, screening for cognitive deficits is not performed regularly in the emergency department (ED). This study aimed to determine factors influencing the frequency of cognitive testing by ED doctors.
Methods
This study included all doctors working in the EDs of three teaching hospitals. A 17-item online survey instrument that collected information on sex, experience, perceived prevalence, perception, and practice of cognitive assessment was distributed through electronic mail and data messaging services.
Results
Of the 210 participants, 72 were male. The estimated mean with standard deviation prevalence of cognitive impairment in older patients in the ED was 39.5%±19.7%. Among the participating ED doctors, 75.8% performed cognitive testing up to 10% of the time. Moreover, the participants ranked cognitive impairment the lowest compared to the other four chronic conditions in terms of its impact on hospitalization outcomes. Multiple linear regression revealed that the doctors’ perceptions of the responsible personnel and the importance of cognitive testing, as well as their lack of expertise, were independently associated with the frequency of testing.
Conclusion
Lack of expertise, perception of the importance of cognitive testing, and lack of consensus on which discipline is responsible for performing cognitive testing in older patients in the ED were the limiting factors in performing cognitive testing in the ED. Improving perception and awareness of the importance of cognitive assessment as a screening tool could improve the detection and overall management of older patients.
INTRODUCTION
With advancements in health services, the population of older adults is growing rapidly in many developing countries. Many people aged ≥65 years enjoy relatively good health. However, these individuals are more likely to have multiple chronic diseases than any other age group, predisposing them to falls, functional decline, vertigo, syncope, urinary incontinence, delirium, and dementia.1)
Cognitive impairment is prevalent among older adult patients in emergency departments (EDs), with reported prevalence rates of 10% to 16%.2-4) However, the curricula of medical courses do not emphasize brief mental status assessments, which has resulted in the inadequate evaluation of older adult patients.5) Cognitive assessment represents one of three significant gaps in the quality of care for geriatrics.6) Screening and measurement instruments to evaluate the mental functions of older patients are often deemed unsuitable for busy and crowded ED settings due to lack of time, staff, space, possible unfamiliarity, or lack of knowledge of the various cognitive screening tools available. As such, cognitive impairment in many patients is overlooked despite its significant influence on patient management and prognosis.7)
Few studies have addressed the relationship between the perception and knowledge of cognitive impairment and cognitive screening in the clinical environment. Therefore, this study examined the relationship between cognitive assessment frequency and ED doctors’ perceptions and attitudes regarding cognitive impairment. The findings of this study will inform future efforts to implement cognitive screening in the ED, leading to enhanced quality of care among older adults presenting in this setting.
MATERIALS AND METHODS
Study Design and Setting
This study applied a cross-sectional survey based on self-administered questionnaires distributed in the EDs of three Malaysian teaching hospitals: University of Malaya Medical Center, Universiti Kebangsaan Malaysia Medical Center, and Hospital Universiti Sains Malaysia. Ethical approval was obtained from the Medical Research Ethics Committee of the University Malaya Medical Center (MREC ID No. 201761-5299). Data were collected over 6 months. All ED doctors in these hospitals were invited to participate in the survey. Doctors from other departments who visited the ED to attend referrals were excluded. Informed consent was waived. This study complied the ethical guidelines for authorship and publishing in the Annals of Geriatric Medicine and Research.8)
Data Collection
This online survey utilized Google Forms (Google, Mountain View, CA, USA). The survey link was disseminated through electronic mail as well as the data messaging services Telegram and WhatsApp to potential respondents from the identified teaching hospitals. Five reminders were sent to non-responders.
Study Instrument
The study instrument comprised a set of questionnaires from a previous study on the knowledge, attitude, and cognitive assessment skills of older doctors in the ED.7) The questionnaire contained 17 items that collected information on clinical experience, sex, level of exposure to older patients, perception and attitude of medical practitioners towards cognitive assessment in the ED, and factors associated with good/bad frequency of cognitive assessment performance in the ED. The survey instrument is included in Supplementary Materials.
Perceptions and attitudes
The respondents were asked to estimate the overall prevalence of cognitive impairment in older patients attending their ED and how frequently they screened patients for this impairment. The doctors were then asked to provide a score out of 10 for conditions that impacted mortality, morbidity, and chances of readmission, where a score of 10 represented the highest level of impact.
Factors influencing cognitive testing
We asked the respondents to indicate the significant factors that limited their ability to perform formal cognitive screening in older patients in the ED, whether they thought it was important and necessary to perform cognitive screening as part of the routine assessment of all older patients in the ED, what the limitations were, and who they felt should perform this assessment. The respondents were asked if they perceived an assessment of orientation as an assessment of cognition, and whether they were familiar with several established cognitive screening tools.
Statistical Analysis
We used OpenEpi Software to calculate a sample size of 128, with a population size of 210 and an anticipated frequency of 30% based on the estimated prevalence of cognitive impairment among older adult patients in the ED reported in several studies.9)
Data analysis was conducted using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics are expressed as means with standard deviations or frequencies with percentages for continuous and categorical data, respectively. We determined the statistical significance of differences between groups using the Mann-Whitney U test and independent t-tests for non-parametric and parametric continuous variables, and the chi-square test for categorical variables, respectively. We then conducted multiple linear regression to identify the factors that independently influenced the likelihood of performing cognitive assessments. The variables identified as significantly different from the baseline comparison were included in the multiple linear regression model in a backward stepwise manner.
RESULTS
Respondent Characteristics
Among 210 potential respondents, 128 (61%) completed the online survey instrument, 72 (56%) of whom were men. Of these, 85 (66%) had at least 3 months’ exposure to geriatric medicine and 120 (94%) had at least 3 months’ experience in the ED, with a response rate of 58.18%. Ninety (70%) had a geriatric medical unit in the hospital. Among the respondents, 10 (8%) were emergency physicians, 17 (13%) were registrars, 31 (24%) were medical officers with >5 years of experience, and 70 (55%) were medical officers with <5 years of experience.
Perceptions and Attitudes
Thirty-one (24%) respondents believed that >60% of older patients in the ED were cognitively impaired. The mean±standard deviation estimated prevalence of cognitive impairment in older adults among patients in the ED was 40±20%, with 19% estimating a prevalence of ≤20%. Sixty-five (51%) respondents felt it was important to perform cognitive screenings in the ED, although 75 (59%) did not feel a simple assessment of orientation to person, place, and time would sufficiently assess cognition. In this study, 102 (80%) and 25 (20%) respondents felt that cognitive assessments should be conducted by the on-call medical team and ED doctors, respectively.
Frequency of Cognitive Screening
Ninety-seven (75.8%) respondents performed cognitive testing up to 10% of the time they assessed older patients in the ED. Less than 5% of the respondents performed more frequent cognitive assessments. Those who perceived cognitive testing in the ED as important (p=0.001) and that it was the doctor’s responsibility to conduct cognitive screening in the ED (p<0.001) were more likely to perform cognitive testing in the ED (Table 1).
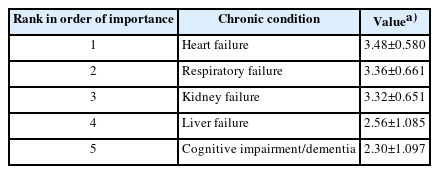
In this study, 106 (83%) respondents identified a lack of time as a factor limiting cognitive testing in the ED, whereas 97 (76%) reported a lack of expertise. Additionally, 66 (52%) reported a lack of availability of screening tools, whereas 42 (33%) responded cited environmental factors and noise levels. Among screening instruments, 102 (95%) respondents had heard of the Mini-Mental State Examination (MMSE) and 76 (59%) had used it for cognitive screening, whereas 59 (46%) and 18 (14%) had heard of or used the Abbreviated Mental Test score, six-item screener, Mini-Cog, CLOX test, short-blessed test, Ottawa 3DY, and AD8 dementia screen. A lack of expertise was significantly associated with a lower frequency of testing (14.3%±14.5% vs. 22.7%±20.7%; p=0.012). Overall, the respondents ranked cognitive impairment as the lowest among the four other medical conditions in terms of its impact on patient mortality, morbidity, and readmission risk (Table 2).
Multiple Linear Regression
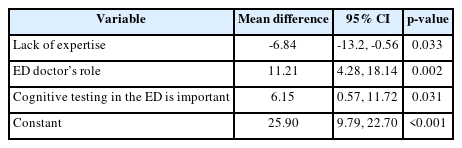
The results of the multiple linear regression analysis (Table 3) revealed that the opinions of the person responsible for conducting the cognitive assessment, the importance of performing cognitive testing in the ED, and the presence of expertise were independently associated with the frequency of cognitive testing. This model explained 18% of the variation in the frequency of cognitive testing in the ED in the study sample (R2=0.18).
DISCUSSION
The results of this study revealed that the frequency of cognitive testing in the EDs of three teaching hospitals in West Malaysia was influenced by previous exposure to geriatric medicine, perception of the importance of cognitive testing in the ED, and attitude towards the responsibility of conducting this testing. Cognitive impairment was ranked the lowest among the conditions that influenced mortality and morbidity in hospitals, and few of the responding doctors had heard of cognitive assessment tools other than the MMSE. The respondents felt that time constraints and a lack of expertise and training were the most important factors limiting cognitive assessment in the ED.
A recent study conducted among older medical inpatients at one of the study centers reported a 27% prevalence of cognitive impairment based on the confusion assessment method,10) a rate lower than the estimated prevalence offered by the respondents. The variation in responses was large, with 25% of respondents overestimating the prevalence as >60%. Despite this overestimation, most respondents conducted cognitive screening <10% of the time, a rate lower than that in a previous study on the frequency of cognitive testing in the ED on different continents.7) This practice may have been influenced by the perception of ED doctors regarding their competency in identifying cognitive impairment in older patients as well as the low priority assigned to cognitive assessment as an organ failure. Overestimation of the prevalence of cognitive impairment suggests an element of preconceived bias or ageism among respondents. This leads to a perception of the limited value of screening and a tendency to ignore older adults in communication and decision-making.
The doctors surveyed in this study lacked familiarity with brief cognitive screening instruments in the ED, despite the availability of several validated brief screening tools designed for the ED setting.11,12) Since there remains no clear consensus in the literature favoring one specific cognitive screening tool over another, EDs may adopt any single screening tool and incorporate it into practice as a routine evaluation of older patients in the ED. The implementation of any brief cognitive screening tool in ED practices and workflows will require the department to ensure adequate staff training in administering and interpreting screening assessments. The Abbreviated Mental Test-4 was introduced as a screening tool for cognition in older patients in the ED in the United Kingdom.13) These good practices could be emulated, and cognitive assessment should be an integral part of the routine clinical workup for all older adult patients in the ED. The frequency of cognitive testing and detection of cognitive impairment may be improved by correcting pre-existing perception biases and ensuring proper training among ED doctors.
Time constraints in the ED due to high patient turnover are a major factor in performing cognitive testing. Adequate doctor training may aid in the selection of appropriate tools and efficiency in conducting cognitive testing, which will reduce the length of time required to administer these tools. Potential environmental issues related to noise levels can be addressed with future planning of the physical infrastructure in terms of ED design and layout. These changes will also enhance privacy and reduce the risk of delirium among older persons in the ED.14) The recognition of delirium is the first step towards its effective prevention and treatment. Effective strategies to reduce the potential for developing cognitive impairment postoperatively have been identified, which further emphasizes the need to detect delirium as it is likely to substantially affect patient outcomes.15)
This study has several limitations. For instance, this study included only teaching hospitals in West Malaysia, although the response rate was superior to that of online surveys conducted among physicians.16) Additionally, a larger survey engaging the help of regulatory bodies or medical societies may help with the national inclusion of other hospital EDs. Future studies are needed to identify effective strategies to enhance cognitive screening in the ED and evaluate interventions to prevent and manage delirium in ED settings.
In conclusion, the frequency of cognitive assessment in the ED is associated with the perception of its importance, the role of the ED doctor, and the ED doctor’s expertise. Measures to change the ED doctors’ perception of the importance of cognitive assessments as part of essential patient care, instituting training to enhance expertise, and providing a suitable screening tool may result in a better cognitive assessment performance in the ED.
Acknowledgements
We thank Dr. Teoh Aik Poey, Dr. Rasidah Ahmad Rosli, Dr. Choo Kim Hoon, and Dr. Yeoh Chun Chiat have assisted in data collection.
Notes
CONFLICT OF INTEREST
The researchers claim no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization, MIZ, TMP; Data curation, SAS; Investigation, SAS; Methodology, MIZ, TMP, AZ; Project administration, SAS, MIZ; Supervision, MIZ, TMP, AZ; Writing-original draft, SAS, MIZ, TMP; Writing-review & editing, MIZ, SAS, TMP, MA.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4235/agmr.23.0150.